Non -standard growth of skin cells is usually called neoplasms.As the main reason for the appearance of neoplasms, experts call the effects of ultraviolet rays.

The second cause of damage to the skin is carcinogenic substances.Behind any new skin education, it is necessary to monitor and consult a doctor - oncologist in a timely manner.
Will perform all the necessary diagnostic procedures.And you will recommend what more actions you will have to perform.
Papilloma, Wart and Condyloma: All this is a consequence of the activity of Papillomavirus or HPV.The virus enters the human body and is inactive for a long time.Under the influence of provocative factors, HPV activation occurs.This is manifested by the formation of soft growth in the skin and mucous membranes.
A neoplasia can worsen the quality of life, its cells are characterized by abuse, which leads to oncology.The timely diagnosis and the treatment of papillomas in the genitals is the key to a healthy and complete intimate life of a woman.
The reasons for the appearance of papillomas in the mouth
The main reason for the appearance of growth in the mouth is the presence of human papilloma in the body.It is easy for them to infect: the virus is transmitted to a domestic way and through personal contacts (touch, unprotected sex).The main methods of infection with the virus:
- Does not complement personal hygiene rules, the use of toilets and dental towels of other people;
- The home method consists of a bad disinfection of objects and utensils used together with an infected person;
- Personal contact with virus bearer (kisses, oral sex, sexual intercourse);
- The infection of the newborn virus occurs during the passage along the child's childbirth channel, which is HPV bearer.
The disease incubation period can last several years.The HPV can only be found by testing.
There are a number of factors that affect virus activation and the appearance of symptoms:
- Frequent colds and chronic inflammatory processes, a decrease in immunity;
- Stressful lifestyle and bad habits;
- Hormonal violations;
- Long -term intake of antibiotics and corticosteroids (hormonal drugs);
- Gastrointestinal tract diseases;
- Pregnancy;
- Systematic lesion of the mucous membrane of the mouth (using toothbrushes with hard bristles, hot food and drink, dentization, orthopedic devices);
- Caries, periodontal disease, gingivitis.
Any papilloma that appeared in the body is caused exclusively by HPV (human papillomavirus).Papillomas in intimate places is a generalized phenomenon.The growth is in the groin, in the vagina, in the member, in the area of the anus.Often, sexual papillomas are found in children.Neoplasias can deliver them to the bearer not only a restriction, but also physical discomfort.According to medical statistics, the Genital Papillomavirus is in almost a quarter of the population.
Papilloma training mechanism in the intimate area
In an inactive state, the sexual virus of human papilloma can live in the body for a fairly long period.The carrier of the virus can infect others, completely unconscious of this.
The viral cell activation and growth process occurs when the body's protective forces weaken.As a result of this, neoplasms occur.
Unlike the generalized opinion that papilloma causes discomfort exclusively in cosmetic terms, it can also cause health problems.
HPV types
According to international standards, all neoplasms are divided into three types:
- Benign.
- Malignant.
- Edge (precancerosos).
It is important to determine the appearance of papillomas in the body.The type of neoplasia depends on virus tension.
In most cases, people face non -hydratic infection, which do not damage health and only cause aesthetic discomfort.It is enough to eliminate such a wart to forget about discomfort.
Distinguishing different types of warts in the body is quite simple when comparing several photos.Each type of education is characterized by a series of characteristics, knowing which is easy to suspect a particular form of the disease.
Ordinary papillomas or vulgar warts
The most common form of Papillomavirus manifestation are ordinary papillomas, popularly called warts.They are caused by several virus strains, which are easily transmitted by contact and sexually.
According to statistics, about each third person on the planet at least once in his life he found the advent of common papillomas.
There are several types of papillomas in the mouth:
- Epithelial hyperplasia: small formations in the form of papillae, more often formed on the sides of the language;
- Simple (vulgar) papilloma appears in heaven and has the form of a flattened cone;
- Vulgar papilloma;
- Grows in gums are more frequently represented in the form of flat papilloma;
- Flat papillomas;
- Cinematographic papillomas have a subtle base, which is often the cause of bleeding and inflammation, if they are injured.They are in a flange flange;
- N Weblomes in the language;
- Acute condylomas have the form of a cone, they are interconnected and form large spotlights;
- Sharmed papillomas

Important!Premature diagnosis threatens the growth of papillomatous nodes in the mucous membranes of the respiratory tract.
Papillomas in the tongue and cheek can have a different form.Polyps on the cheek are a small soft bump and do not cause pain.Language growths are subject to irritation and micro-hierba, which can cause bleeding.
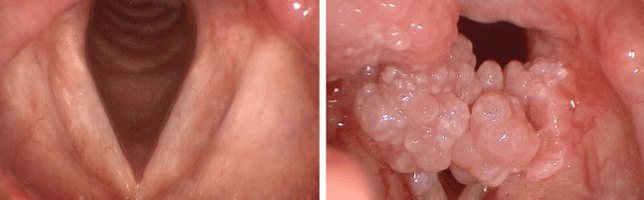
Papillomas in the tonsils are often confused with laryngitis or purulent throat pain.Due to the growth, the swelling of the respiratory tract and the vocal strings can be observed, which causes difficulty breathing.
Unpleasant sensations accompany the food absorption process, even liquids.Sometimes a person experiences the presence of a foreign body in the throat.
The appearance of papillomas in the larynx can be accompanied by changes in the voice, respiratory problems.During the consumption of solid foods, the mucous membrane with growth can be crushed.The red throat in the child can indicate the presence of growth.Papillomatosis of larynx in children is the cause of bronchitis.
The appearance of cone or polyp -shaped pathological formations in the gum (gum growth) is dangerous, since the mucous membrane will be injured by a toothbrush or post -tiny dentures.Ultimately, this will lead to an inflammatory process and an infection of unpaid sores.
Papillomavirus, in addition to skin changes, is a danger to the development of various diseases.The type of infection shows how the danger will develop and what is.
The determination of the type of condil is necessary for:
- Identification is a risk of growth in a malignant tumor;
- Effective treatment selection;
- Determine the type of infection.
Simple
Also known as vulgar or ordinary.Papilloma formation is preceded by a slight ardor sensation.
Over time, a spherical growth appears, which resembles a tumor.Even later, the smooth surface of the neoplasia changes to the roughness, and the color of the body passes to darker.
The dimensions can vary from 1 to 10 mm.
Most of the time, ordinary warts between the fingers and palms of the rear appear.In children who move mainly, they can be located on his knees.They are single and multiple.
Often, vulgar papillomas do not represent danger to human health, which represents benign growth.
Subanary
The name itself indicates the location of papillomas.In order not to confuse them with calluses, there are a number of speech signals:
- Neoplasia in all signs resembles an ordinary wart;
- There is pain in the growth area when using small shoes;
- There is no leather pattern, and the surface is rough.
Papillomatosis of inherent mosaic plantar vertrucas, when bubbles are formed near basic formation, over time: papillomas.
In young children, plantar warts can disappear on their own.
Department
They have an oval shape, stretched, less round.They are characterized by a slight height, only a few millimeters stand out on the skin.The face is affected, the skin of the upper part of the chest, sometimes the external genital organs.
The color is slightly darker than a body dye.Nearby, the Papillomas Airplanes have the property of connecting to one place, after which they become much more notable.
Movie
The warts characterized by a specific leg and a longitudinal shape are called threaded (Acrocordus).Initially, lower neoplasia has the shape of a small cone, which soon stretches.
Most of the time they are in men and women after 40 years.They are located on the neck, on the eyelids, under the armpits, in the inguinal area, near the mammary glands.Often injured due to the presence of a thin leg, which is easy to damage with clothes or an inaccurate movement.
Sharp
Externally, it resembles papillary education.They can affect the skin both by one and in complete groups.As they develop, they combine in a single whole, forming a bright pink meat or pink.
The appearance of pointed warts is caused by a sexually transmitted infection.In this sense, condylomas affect the genitals, the inguinal zone, the area near the anus.
Sharp papillomas develop very quickly and can occupy an extensive part of healthy tissues in a few days.Even after a successful treatment, relapse is not excluded.
Medicine has more than one hundred varieties of papillomavirus.Around forty of them are transmitted sexually and, consequently, affects the genitals of men and women, many types of HPV do not damage at all, some are especially dangerous and can cause oncological diseases.
Human papillomavirus types are common to classify by the degree of probability of the formation of cancer formations in the skin.Distinguish:
- A particularly dangerous guy: 16, 18, 36, 45;
- The average danger type is 31, 33, 35, 51, 52, 58;
- SAFE TYPE - 6, 11, 42, 43, 44.
HPV is a microorganism with up to one hundred stamps.Depending on the type that affects the person of the HPV label, different types of papillomas are also formed in the skin.They differ in appearance, growth rate, body location.
Some papillomatous growths are detected in the mucous membranes of the oral cavity, in the bladder, in women in the vagina and in men in the penis.
The determination of the papilloma species is necessary to select the most effective treatment method and evaluate the risk of rebirth of this tumor in malignant.
Official medicine divides HPV into 4 groups:
- not oncogenic;
- oncogenic;
- Average cancer risk transport;
- characterized by a high degree of carcinogeicits.
Not oncogenic, that is, they do not reborn in a tumor of cancer over time, as a rule, they are papillomas of the vulgar, flat and planting type.If we take the general definition of Papilloma, then, translated from Latin, it can characterize it as a "papilla -shaped tumor."















